You may have heard the term “wet brain” in connection with long-term, heavy alcohol use. It’s a colloquial term for the medical condition Wernicke-Korsakoff syndrome. This brain disorder refers to two separate conditions that often occur together. The first stage is Wernicke encephalopathy, then Korsakoff syndrome can develop after the symptoms of the first disorder begin to lessen.
What exactly is wet brain syndrome? How can you recognize the signs of wet brain? What does wet brain treatment involve? Take a closer look at Wernicke-Korsakoff syndrome to understand how it develops and what can be done once it does.
What Is Wet Brain, and How Does It Occur?
Wet brain goes by many different names, such as Wernicke-Korsakoff syndrome, alcohol dementia, alcoholic encephalopathy and Korsakoff psychosis. Thiamine, or vitamin B1, deficiency causes this neurological condition.
Vitamin B1 is a vital nutrient for maintaining a healthy nervous system and brain. The body is unable to produce thiamine on its own. Instead, vitamin B1 is naturally contained in foods like whole grains, beef, pork, potatoes and kale.
Excessive chronic alcohol use can affect how the body absorbs vitamin B1, leading to deficiency. When the brain does not have enough thiamine, it struggles to convert sugar into the energy it needs for normal, healthy function. This deficiency is what causes the development of wet brain. The condition damages parts of the brain responsible for movement and coordination.
Thiamine deficiency can happen relatively quickly — it is possible to reach deficiency within a month. The lack of adequate thiamine can cause brain bleeding associated with wet brain.
If left untreated, these conditions can cause permanent damage to parts of the brain responsible for memory and other areas, including the:
- Brain stem
- Cerebellum
- Hypothalamus
- Thalamus
- Mammillary bodies
Wet brain is not always easy to diagnose, particularly if the patient is confused or unable to share accurate medical history. If someone has a history of alcohol misuse, physicians may look for signs of damage to the liver and conduct tests to determine the levels of vitamin B1 in the body. In addition to conducting a physical examination, doctors may also order imaging tests to look for damage to the brain. The patient must be sober to be diagnosed with Wernicke-Korsakoff syndrome, though.

Who Is Most at Risk of Developing Wet Brain?
Wet brain is not a genetic disease. Rather, it develops due to lifestyle factors and other health conditions that result in insufficient thiamine intake and absorption. Risk factors for Wernicke-Korsakoff syndrome include:
- Alcohol addiction: Alcohol addiction is the most common cause of wet brain. Excessive alcohol consumption over long periods can make it difficult for the body to absorb thiamine properly. Additionally, people struggling with alcohol addiction may be more prone to poor diet and malnourishment. They may not be consuming enough vitamin B1, and their bodies can’t absorb the small amounts they do consume.
- Malnourishment: Alcohol addiction is not the only condition that can cause malnourishment. Eating disorders, such as anorexia, are associated with a higher risk of developing Wernicke-Korsakoff syndrome.
- Kidney dialysis: People who are undergoing kidney dialysis may also be at risk of poor vitamin B1 absorption, which can eventually lead to wet brain. Kidney dialysis is necessary for people who have chronic kidney disease.
- Acquired immunodeficiency syndrome (AIDS): AIDS can increase the risk of many health conditions. Research has shown that this condition can cause thiamine deficiency.
- Aging: As we age, it becomes difficult for our bodies to absorb nutrients. Aging individuals may not consume foods rich in vitamin B1, either.
What Are the Early Symptoms of Wet Brain?
There are two stages of wet brain — Wernicke encephalopathy and Korsakoff syndrome. Without quick recognition and treatment of early symptoms associated with Wernicke encephalopathy, the condition could develop into Korsakoff syndrome. The early signs of wet brain can be confused with the effects of alcohol consumption, but someone with wet brain will experience symptoms when they are sober.
The early signs of alcoholic wet brain include:
- Lack of coordination and weakness: The damage done to the brain will affect an individual’s coordination and ability to move. Someone with wet brain may struggle to maintain their balance and exhibit muscle weakness and impaired reflexes. This symptom is also known as ataxia.
- Confusion: Because of the damage to the brain, someone with this condition may exhibit signs of confusion. That confusion could make daily tasks a challenge or lead to a loss of interest, apathy and agitation.
- Changes in heart rate and body temperature: The early stage of wet brain can cause physical symptoms with a racing heart rate and raise body temperature.
- Vision changes: In the early stages of wet brain, you may see someone exhibit odd eye movements. The person’s eyes may be moving laterally or up and down. They may experience double vision or have a drooping eyelid.
What Is Wernicke Encephalopathy, and What Are Its Symptoms?
Wernicke-Korsakoff syndrome takes the first part of its name from Wernicke encephalopathy. This condition is separate from Korsakoff syndrome, although the two are closely linked and usually considered different phases of Wernicke-Korsakoff syndrome. Wernicke encephalopathy presents as the early symptoms of wet brain mentioned above, and it’s an acute, short-lived condition. If you recognize any of those early symptoms in a loved one who struggles with alcohol addiction, help them seek immediate treatment.
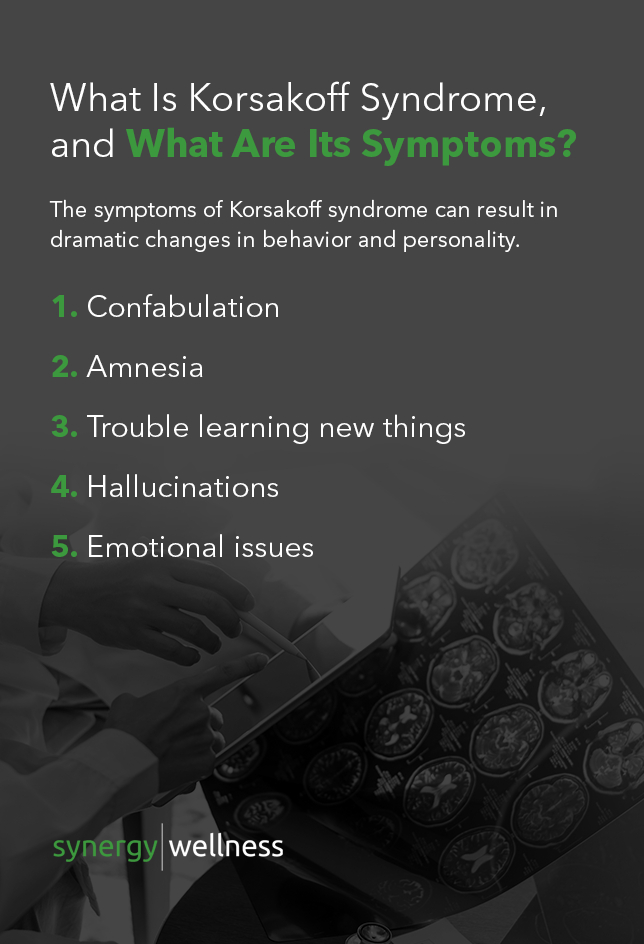
What Is Korsakoff Syndrome, and What Are Its Symptoms?
While Wernicke encephalopathy does not always lead to the second stage of Wernicke-Korsakoff syndrome, about 80 to 90 percent of alcoholics who experience this stage will develop Korsakoff syndrome. It’s is a chronic condition that can develop if Wernicke encephalopathy is not treated promptly.
The symptoms of Korsakoff syndrome can result in dramatic changes in behavior and personality. The signs of wet brain in its second stage include:
- Confabulation: Confabulation is a type of memory error and an early sign of Korsakoff syndrome. Someone experiencing this symptom is prone to giving untrue, exaggerated or muddled versions of events due to their condition. But these statements aren’t intentional lies. The confabulations are often convincing and can be hard to recognize as a symptom, but they often come from a place of confusion or memory loss.
- Amnesia: When wet brain progresses from Wernicke encephalopathy to Korsakoff syndrome, a person’s memory is impacted. Retrograde and anterograde amnesia are common during the second stage. Retrograde amnesia is a difficulty remembering events before the onset of the condition, while anterograde amnesia is a difficulty storing new memories after the onset of Korsakoff syndrome.
- Trouble learning new things: Confusion and memory issues can result in difficulty learning new things. That symptom, in itself, can cause additional frustrations to the agitation someone in the first stage of wet brain may experience.
- Hallucinations: Hallucinations, or sensory experiences that feel very real but are a product of the mind, are common during the second stage of wet brain. Someone with this condition may hear or see things that aren’t there, which may contribute to confabulations.
- Emotional issues: Difficulty regulating emotions is another common symptom of Korsakoff syndrome. Those in the second stage of wet brain may have a lack of response to events happening around them, or they may experience sudden or unexplained euphoria.

Is Wet Brain Permanent?
Is wet brain reversible? The answer to this question depends on how far the condition has progressed. The first stage of wet brain, Wernicke encephalopathy, is an acute condition. Early intervention during this stage can help to reverse those symptoms. If the diagnosis is made in time and treatment is administered, it’s even possible to completely resolve early symptoms. But, if left untreated, Wernicke encephalopathy can progress to the second stage. Treatment often involves hospitalization and significant, long-term lifestyle changes.
When wet brain enters its second stage, the condition becomes much more difficult to treat. It is rare for the symptoms of Korsakoff syndrome to completely resolve. In most cases, treatment focuses on supportive care.
The neurological symptoms associated with the second stage of wet brain are likely to continue in some form indefinitely. Patients may see some improvement in vision and balance once treatment begins, but memory issues can persist. Approximately a quarter of people who develop Korsakoff syndrome will recover, while 50% will make some progress but not reach full recovery. The remaining quarter will experience no change in their symptoms.
Wet brain life expectancy is an important consideration when considering its permanency. Alcohol addiction, even if it has not progressed to the point of Wernicke-Korsakoff syndrome, can considerably decrease life expectancy. Research has shown that people who are hospitalized for alcohol misuse die 24 to 28 years sooner compared to people in the general population.
Following an experience with Wernicke-Korsakoff syndrome, it is possible someone could still have a normal life expectancy. To achieve that, they’d need to make lifestyle changes and stop drinking alcohol. If left completely untreated, Wernicke encephalopathy can be fatal in about 10 to 20% of people. With treatment, though, the prognosis for those with Wernicke-Korsakoff syndrome can be better than other conditions, like Alzheimer’s.
Can Wet Brain Be Treated?
Wet brain from alcohol requires treatment as soon as possible. Initial treatment for this condition includes:
- Thiamine: Thiamine is the first step in getting treatment for both stages of wet brain. In many cases, the thiamine is administered intravenously to the patient. It is also possible that the patient will be prescribed oral thiamine to take after being released. Continued use of the oral supplements may need to last as long as the person continues to consume alcohol.
- Hydration: If someone is admitted to the hospital with the symptoms of wet brain, they may also require hydration support.
People who have experienced wet brain, in either its first or second stage, will also be given the recommendation to make lifestyle changes, including:
- Abstinence from alcohol: Reducing or eliminating alcohol intake is the most critical change to make following an experience with wet brain. Continued alcohol misuse can perpetuate thiamine deficiency and increase the risk of developing Wernicke-Korsakoff syndrome again. Anyone experiencing wet brain due to excessive alcohol consumption should change their relationship with drinking as a long-term strategy.
- Healthy diet: Malnourishment can play a significant role in developing thiamine deficiency. As a part of treatment, doctors will likely recommend adopting and maintaining a healthy and balanced diet. They’ll work to ensure the patient consumes enough vital nutrients, particularly vitamin B1.
- Nutritional supplements: While a balanced diet is always a good lifestyle choice, people who have had wet brain and are at risk of developing it again may need to take nutritional supplements. Doctors will evaluate the patient’s current diet and make recommendations for supplements to ensure their body gets every nutrient it needs, including thiamine.
Depending on a patient’s prognosis, care may need to be supportive and focused on managing symptoms. For example, patients with severe memory impairment or confusion may need to receive care in a long-term residential facility.
How Rehabilitation for Alcohol Use Can Help
Early intervention is essential when you or a loved one is at risk of developing or already has Wernicke-Korsakoff syndrome. Continued misuse of alcohol increases the risk of worsening this condition or developing it again. Additionally, Korsakoff syndrome can lessen a person’s alcohol tolerance, which increases the risk for other health concerns related to alcohol consumption. Rehabilitation for alcohol use can help people break the cycle of addiction and receive the supportive care they need.
Rehabilitation for alcohol use does more than help lower the risk for worsening or developing Wernicke-Korsakoff syndrome. This support offers people:
- A safe environment: If someone wants to quit drinking, doing so on their own can be dangerous. Rehabilitation programs offer a safe environment with professionals who are trained to help patients safely go through the withdrawal and detox process. The staff at these programs will help you without judgment.
- A support network: Addiction can be scary and lonely. Rehabilitation introduces individuals to a network of people who are there to help them through the recovery process. That support network can help patients through any relapses and celebrate successes. Patients do not need to go through the recovery process alone.
- Tools for long-term recovery: Rehabilitation is about more than achieving initial sobriety. These programs are designed to give patients the tools they need to achieve long-term recovery. Services like individual counseling and group therapy can help build the resources patients need to understand and break their addictions.

Learn About Personalized Addiction Treatment at Synergy Recovery
Alcohol addiction is a difficult cycle to break without help. Everyone’s experience with addiction is different, and a one-size-fits-all approach to treatment is not the answer. At Synergy Recovery, we treat you as an individual with unique needs. Our treatment approach uses a combination of medication and counseling. We work with you to build a treatment plan that will help you find the path to long-term recovery.
If you or a loved one is struggling with alcohol addiction, we are here to offer nonjudgmental and professional care. Contact us to schedule an appointment and get the help you need.