When taking extended-release prescription medication, it’s essential to look into its drug interactions and potential side effects. Unlike an immediate-release drug, when you take an extended-release medication, it gradually enters your system throughout the day. This allows you to take medicine less frequently and reduces the risk of overdose.
Extended-release opioids are among the most common types of extended-release drugs. If you take opioids with food or alcohol, you could potentially experience a phenomenon called “dose dumping.” We’ll discuss the causes of dose dumping below, as well as common dose-dumping side effects and some treatment methods if you or a loved one suffers from alcohol or opioid addiction.
What Is Dose Dumping?
Understanding drug metabolism will help you understand how dose dumping occurs. When we ingest drugs, the enzymes in our body break them down to cause a specific reaction. The rate of drug metabolism determines the length and intensity of the drug’s response in our bodies.
Dose dumping refers to the phenomenon that happens when an extended-release drug enters the body too rapidly. The quick-release can occur with any oral dosage form, from pills and capsules to tablets or liquid solutions.
While some drugs are labeled as having a slow-release rate, they have the potential to release rapidly with the introduction of certain environmental factors. Most notably, when taking extended-release opioids with food or alcohol, the effects of the drug can intensify and cause dose dumping.
Most drug companies try to avoid drugs with these potential effects. Certain prescription pain medications have been pulled from the market for their dose-dumping effects once taken with alcohol, including Palladone Once Daily, an opioid used to treat moderate or severe pain.

What Causes Dose Dumping?
Food, alcohol and mixing opiates with other depressants or stimulants can cause dose dumping. While many opioids are designed for a delayed reaction, alcohol dose dumping occurs when the drug is released quickly or all at once, causing adverse effects on the user.
Dose dumping is more commonly noted when patients take drugs orally that digest in the gastrointestinal tract. Around the time you take your medication, you might also ingest fatty meals or alcohol that could increase drug delivery. These substances can either speed up the drug release rate or stimulate your body’s absorption process to increase its rate of drug uptake.
Dose dumping opioids include morphine, hydromorphone, oxycodone, tramadol and dihydrocodeine. You should always be careful to read the warning labels on your prescription drugs and watch out for the susceptible opioids to prevent dose dumping from happening to you or someone you know.
Alcohol-Induced Dose Dumping
The release rate of a drug is controlled by a film coating or matrix made of polymer. Since alcohol is a solvent and polymers are highly soluble, they’ll dissolve in the presence of alcohol. This effect can cause alcohol-induced dose dumping.
Alcohol-induced dose dumping gained attention in 2005 when Palladone produced dose-dumping effects on users. This extended-release form of hydromorphone, an opioid painkiller, contained high soluble polymers that dissolved when taken with alcohol, causing the FDA to discontinue it.
Food-Induced Dose Dumping
Like alcohol, some foods — particularly fatty foods like meat and dairy — can damage the drug’s release-controlling polymers or speed up drug absorption. Both of these effects can cause dose dumping. It can also occur from foods that produce pH variability in the gastrointestinal tract.
A popular drug product linked to food-induced dose dumping is theophylline, meant to treat asthma and lung issues. For this reason, people take it on an empty stomach just once a day.
The Dangers of Alcohol-Induced Dose Dumping
Many people unknowingly take prescription painkillers with alcohol without realizing the safety risks posed by mixing the two intoxicants. It’s essential to understand how these different drugs interact to prevent yourself or someone you know from accidental dose dumping.
Common painkillers or prescription opiates include:
- Opana
- Fentanyl
- Oxycontin
- Vicodin
- Codeine
Since these opiates are highly effective at reducing pain, they’re often overprescribed, leading to drug abuse and a higher potential for dose dumping.
Prescription painkillers have time-release additives that make them safe to take over a long period under doctor supervision — however, drinking beer or having a glass of wine with your medication or within two hours of taking opioids increases the level of narcotics in the body.
When mixing opioids with alcohol, patients can experience several short-term and long-term health risks, including:
1. Liver Damage
While alcohol can increase the number of narcotics that enter the body, opioids can increase how alcohol affects the body. When taken together, you have a higher risk of liver damage, cirrhosis or liver failure.
Specific prescription opioid painkillers like Percocet and Vicodin contain acetaminophens. When used alone, acetaminophen is a non-steroidal anti-inflammatory drug (NSAID) safe for pain relief. However, many people have overdosed by taking acetaminophen alongside their opioids for additional relief. Since acetaminophen can harm the liver if taken too often, the risk of liver damage increases when coupled with opioids containing the drug.
2. Memory Loss
Opioids can interfere with the formation of new memories, especially when taken at high doses. Opioid painkillers bind to opioid receptor cells in the brain and block one’s emotional reaction to pain. The emotional pathways are associated with memory formation and, once blocked by opioid use, can increase your risk of memory loss the longer you take them.
Similarly, binge drinking can increase the risk of blackouts and memory loss. High blood concentrations prevent short-term memories from being stored in long-term memory. When combined with prescription painkillers, you can experience decreased motor function over time and dementia-like symptoms as they increase each other’s damaging effects.
3. Decreased Effectiveness
The main advantage of extended-release medication is its effects last a long time, so you only need to take them once or twice a day. Dose dumping can remove this benefit by causing the drug’s effects to wear off more quickly.
4. Increased or Worsened Side Effects
Since dose dumping causes drugs to enter your system more rapidly, it can increase or worsen the drugs’ side effects or cause drug-induced toxicity.
Side effects vary between the different extended-release medications and opioids. Common ones include:
- Nausea
- Constipation
- Fatigue
- Dizziness
- Vomiting
5. Increased Risk of Overdose
Opioid overdose becomes lethal when the central nervous system is suppressed from the use of sedating substances like alcohol. Users might experience an elevation of side effects like sedation, drowsiness or depressed respiratory function, making dose dumping a huge safety concern.
The central nervous system controls heart rate, breathing and other pertinent bodily functions. By combining opioids and alcohol, you can double the effects of both, which can cause an overdose.
With an overly depressed central nervous system, you can experience slow breathing that can stop altogether. It can also lower the oxygen reaching your brain and cause brain damage, coma or death.
Mixing opioids with other depressants like alcohol, whether intentionally or unknowingly, has contributed to the rising number of opioid overdose deaths in the U.S. In 2017, the highest rate of fatalities from alcohol-induced overdoses occurred with heroin or synthetic opioids such as methadone or fentanyl.
Symptoms of drug overdose include:
- Nausea and vomiting
- Chest pain
- Seizure
- Anxiety or irritability
- Confusion
- Cold, clammy skin
- Shallow or irregular breathing
- A change in pupil size
- Bluish lips or fingernails
- A rapid change in body temperature
- Loss of consciousness
- Slow or irregular heartbeat
- Vision impairment
If you or someone you know experiences these symptoms, it’s essential that you seek emergency health care services right away. If left untreated, an overdose can be fatal.
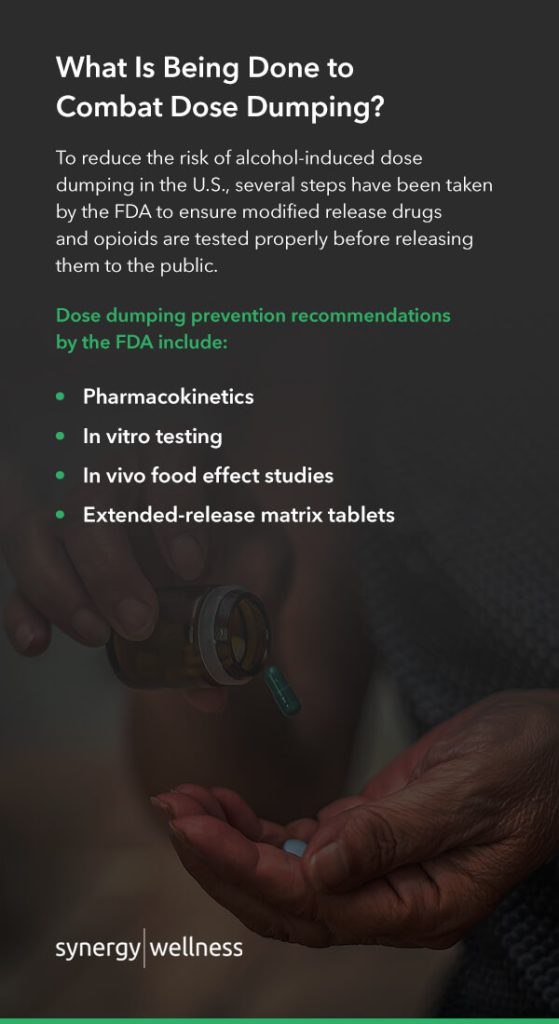
What Is Being Done to Combat Dose Dumping?
To reduce the risk of alcohol-induced dose dumping in the U.S., several steps have been taken by the FDA to ensure modified release drugs and opioids are tested properly before releasing them to the public. Dose dumping prevention recommendations by the FDA include:
- Pharmacokinetics: Pharmacologists study the movement of opioids within the body to determine how to prevent dose dumping. They look at how the drug is absorbed, how it distributes across the body, how it metabolizes and the effects caused by the introduction of food and alcohol to assess patients’ risk.
- In vitro testing: Colloquially referred to as “test-tube experiments,” medical scientists test extended-release formulations for in vitro dissolution to see how opioids react to certain environmental factors.
- In vivo food effect studies: Medical scientists also study how the opioid performs in the human body once taken with food before releasing it to the public. This provides a more reliable assessment of how the drug will perform and interact with other substances.
- Extended-release matrix tablets: The FDA also recommends the release of matrix tablets to deter opioid misuse and addiction and prevent dose dumping, such as reformulated OxyContin, Hysingla ER, Targibiq ER, Xtampza ER and Embeda. These drugs are designed to resist chemical and physical manipulations.
Treatment Methods for Alcohol and Opioid Addiction
Treatments for alcohol and opioid addiction overlap in many ways. Both can involve detox, inpatient or outpatient counseling, peer support groups and medicines that help curb addiction and get you started on a successful recovery plan.
Further, while in treatment for either addiction, you might opt for spiritual or religious practice to help you gain insight into your spiritual side to help you recover.
We’ll provide an overview of options to help you or someone who may be struggling.
Treatment for Alcohol Use Disorder
Depending on your needs, treatment might involve a brief intervention, group or individual counseling or an outpatient or inpatient residential stay. The goal of treatment is to stop alcohol use and improve your quality of life.
Treatment methods include:
- Detox and withdrawal: Treatment might begin with a medically managed detox program at an inpatient center or hospital. This can take two to seven days and might require sedating medications to prevent withdrawal symptoms.
- Establishing goals: Specialists will usually set goals and behavior-changing techniques to help treat patients with alcohol use disorder. They might also employ self-help manuals and follow-up care at a treatment facility.
- Psychological counseling and treatment: Therapy and counseling in a group setting or on your own can help you understand your problem and receive support for the mental aspects of alcohol use. Cognitive treatment through medication or therapy can help you cope with disorders that occur alongside alcohol use disorders like anxiety or depression.
- Oral medications: The drugs Disulfiram or Antabuse can help prevent you from drinking. It won’t cure your disorder or remove your compulsion to consume alcohol, though it can produce a physical reaction to block the good feelings alcohol produces. This can help curb cravings so you’re less prone to excessive drinking.
- Injected medications: Similar to oral medications, health care professionals can inject a drug called Vivitrol into your body once a month to help you recover from alcohol use disorder.
- Continued support: Support groups and aftercare programs can help you continue down your recovery path and manage relapses and the life changes caused by treatment and addiction.
Treatment for Opioid Addiction
Depending on the patient, treatment for opioid addiction might involve:
- Medicines: Like alcohol use disorder, one can take medicines to treat opioid addiction. These medicines can decrease withdrawal symptoms and cravings to help you heal. Common ones include suboxone, methadone, buprenorphine and naltrexone.
- Medication-assisted therapy: This type of therapy can involve medication, counseling and behavioral therapy. An all-encompassing program with a well-rounded plan can help increase recovery success.
- Counseling: Therapy or individual counseling can help you change your attitudes and behaviors associated with drug use. Like alcohol misuse treatment, you can learn more about how mental health issues impact or result from opioid addiction. You can also build healthy life skills to take with you after treatment. Group counseling can help you feel like you are not alone since you can share your issues with those facing similar challenges.
- Residential treatment: Residential programs combine treatment with housing. In a residential treatment center, you’ll live with peers and support one another in your path to recovery.
- Hospital-based care: In-patient hospital programs combine addiction treatment and health care services for those with medical problems. Hospitals can also offer structured intensive outpatient treatment that involves medicines, counseling and behavioral therapy.
Treatment for Opioid and Alcohol Addiction in Bakersfield, CA
If you or someone you love is struggling with opioid or alcohol addiction, outpatient care can help break the cycle. At Synergy Wellness, we foster an environment of nonjudgement and discreteness to help you through your addiction and improve your quality of life. Our specialists use a combination of counseling and prescription medications such as Vivitrol or Suboxone to assist you through the process.
You’ll receive the care and respect you deserve with a treatment plan designed for you. If you’ve attempted alcohol use disorder treatment in the past and found it unsuccessful, our intensive partial hospitalization plan involves five a day, six-hour sessions to treat your addiction.
We also have flexible outpatient and individual counseling options for your needs, whether you’re struggling with opioid addiction or alcohol use disorder. With outpatient services, you can receive daytime care and leave at night so you’re still surrounded by friends and family throughout your recovery.
To learn more about our treatment services, contact us today!